Published online Aug 6, 2014. doi: 10.5527/wjn.v3.i3.114
Revised: April 28, 2014
Accepted: May 28, 2014
Published online: August 6, 2014
Epiploic appendagitis (EA) is rare cause of acute or subacute abdominal pain in patients on peritoneal dialysis (PD), where the diagnosis can be challenging as the clinical features, laboratory markers and imaging characteristics have not been described previously in this group of patients. Here, we present the management of a case of EA in a patient on PD and review published literature pertinent to the subject. The importance of establishing the diagnosis early by laparoscopy is emphasised.
Core tip: The diagnosis and management of a patient with epiploic appendagitis (EA), who presents with acute abdominal pain, can be challenging. A high index of suspicion, exclusion of other causes of acute abdominal pain by computerised tomographic scan and an a low threshold for an early diagnostic laparoscopy is the way forward in establishing the diagnosis of EA and preservation of peritoneal dialysis catheter.
- Citation: Shrestha B, Hampton J. Recurrent epiploic appendagitis and peritoneal dialysis: A case report and literature review. World J Nephrol 2014; 3(3): 114-117
- URL: https://www.wjgnet.com/2220-6124/full/v3/i3/114.htm
- DOI: https://dx.doi.org/10.5527/wjn.v3.i3.114
Epiploic appendagitis (EA) is a rare cause of acute or subacute abdominal pain, where the diagnosis can be challenging, particularly in a patient on peritoneal dialysis (PD)[1]. Lack of pathognomonic clinical, laboratory and radiological findings can pose significant difficulty in diagnosis and differentiation of EA from common acute abdominal pathologies. EA is a self-limiting condition with a benign clinical course, which can be managed conservatively, if the diagnosis can be made through exclusion. A Medline search on the management of EA on PD patients showed no publications on this subject. Here, we present the management of patient on PD presenting with left iliac fossa pain (LIF), where the diagnosis of EA was confirmed by laparoscopy and review the pertinent published literature.
A 61-year-old female, who was on peritoneal dialysis for 2 years for renal failure secondary to Escherichia coli sepsis in the past, had presented with sudden onset of continuous severe LIF in the early hours of the morning which was exacerbated by movements. There was no associated fever, vomiting, change in bowel habit or haemodynamic instability. There was marked tenderness and guarding in the LIF inferolateral to the exit site of the PD catheter. However, there was no clinical evidence of infection involving the exit site, catheter tunnel or peritonitis. The complete blood count was normal, but the C-reactive protein (CRP) was raised to 16 mg/L (normal range, 0-5 mg/L). The cytology of PD fluid showed a white blood cell count of 251/mm3 with 94% polymorphonuclear leucocytes with negative culture. An ultrasound (US) scan and a non-contrast computerised tomographic (CT) scan of abdomen were unremarkable. She was treated with analgesics, intraperitoneal Vancomycin (2 gm) and Gentamicin (32 mg) on a presumed diagnosis of low-grade peritonitis. Five days later her abdominal pain had subsided significantly, hence she was discharged home.
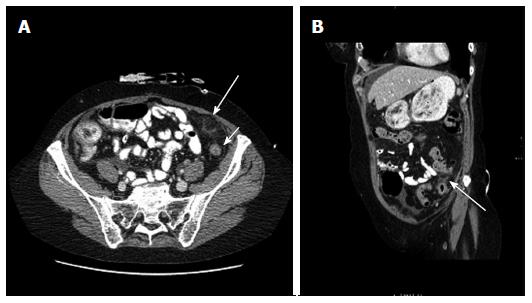
Two weeks later, she presented with recurrent pain in the LIF, which on one occasion was very intense mimicking acute mesenteric ischaemia requiring repeated administration of morphine. Abdominal examination revealed tenderness and guarding in the LIF. The white cell count was normal, but the CRP was elevated to 67 mg/L. The culture of the PD fluid was sterile. Arterial blood gas and blood lactate were normal. A repeat contrast enhanced CT scan of abdomen showed patent coeliac axis, superior and inferior mesenteric arteries with normal perfusion of the intestine. However there was small amount of fluid in the pelvis and a fat density area with some surrounding inflammation anterior to the descending colon in the left iliac fossa just below the abdominal wall, which was suggestive of the possible diagnosis of epiploic appendagitis (Figure 1). A flexible sigmoidoscopy and transvaginal US scan were normal.
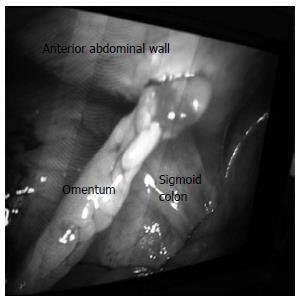
As the abdominal pain was intractable and persistent after 6 wk of treatment, under general anaesthesia, the PD catheter was removed and a laparoscopy was carried out using the PD catheter entry site. The greater omentum was adherent in the LIF where a small area on the anterior surface of the middle of the sigmoid colon was adherent to anterior abdominal wall over the site of maximum tenderness. There was evidence of inflammation on the anterior surface of the sigmoid colon where appendix epiploicae were present at the site of fibrinous adhesion, indicating epiploica appendagitis (Figure 2). Rest of the sigmoid colon and the abdominal organs were normal. The adhesion was released laparoscopically after inserting a 5 mm port in the right iliac fossa and a new PD catheter was replaced. This led to complete resolution of symptoms and restoration of PD.
Epiploic appendages are peritoneal outpouching of adipose tissue on the colonic surface, 50-100 in number, measuring 0.5-5 cm in length. The majority of them are situated on the sigmoid and descending colon, which explains the preponderance of EA in the left side of the abdomen, compatible with the finding in our case. Each appendage is supplied with one or two arteries from the colonic vasa recta and drained by a single vein[2]. These vascular structures are extremely mobile and susceptible to ischaemia, inflammation and necrosis if torsion, kink or stretching occurs[3].
Since the first report of EA in 1959 by T Case, several case series have been described in the normal population[4], but the clinical features and management of EA in a PD patient has not been reported previously. The primary EA is believed to occur spontaneously, whereas secondary EA occurs as a result of adjacent inflammatory diseases such as diverticulitis, appendicitis and cholecystitis[5,6].
The presenting symptom of EA is a localised non-migratory pain on the LIF, in the absence of severe illness, which is exacerbated by movements. Localised and rebound tenderness are usually present. There is lack of significant inflammatory response, particularly at the time of initial presentation. In PD patients, the nature of pain may be different if the inflamed appendage is adherent to the parietes and repeated distension of the abdominal wall during PD fluid exchanges may lead to stretching of the sensitive parietal peritoneum and severe pain. A high index of suspicion of EA after exclusion of acute diverticulitis, appendicitis, haemorrhagic ovarian cyst, torsion of an ovarian cyst, pelvic inflammatory diseases and mesenteric lymphadenitis, delayed perforation of bowel by the PD catheter or ischaemia of intra-abdominal organs, is necessary. Epiploic appendagitis adherent to the abdominal wall can lead to complications such as intestinal obstruction form torsion of the small intestine, strangulation, ileus and catheter drainage problems[7-10].
The patients on PD are more prone to serious intra-abdominal pathology than patients on haemodialysis due to an effect of PD to impair the normal physiological response of the peritoneal membrane[11]. An early diagnosis of EA by excluding all causes of surgical peritonitis is paramount in PD patients. An undiagnosed peritonitis in PD patients caused by perforation of intestine or intestinal ischaemia can prove fatal. The presence of pneumoperitoneum visible in erect chest-X-ray and CT scan may not be sensitive or specific for a perforated hollow viscus since this may be present in 3.7% of healthy PD patients and in 0%-11% in patients with bowel perforation[12].
Laboratory findings specific to EA could be insignificant according to several studies. Mild leucocytosis and a low-grade increase in CRP is accepted as markers of mild inflammation[13]. The diagnostic yield of radiological investigations such as US, CT and magnetic resonance (MR) scan is considered to be high, although the findings are not specific for EA. Epiploic appendages cannot usually be seen during radiological imaging unless inflamed or associated with gross ascites or haemoperitoneum. EA may be diagnosed with US scan, with findings of solid, oval, non-compressible hyperechoic mass under the site of maximal tenderness, and lack central blood flow on Doppler US scan[14]. The CT features of EA are characteristic according to several studies, which show a pericolonic ovoid mass with hyperattenuating rim surrounded by fat stranding[15,16]. The anterior localisation of EA in relationship to the colonic lumen is mentioned as a usual finding in making a confident diagnosis. The other fatty lesions that can mimic US and CT findings of acute EA are chronic calcified EA, omental infarction, post-operative changes, and peritoneal carcinomatosis[17,18]. The MR scan findings include an oval shaped fat intensity mass with a central dot on T1- and T2-weighted images, which possessed an enhancing rim on post-gadolinium T1-weighted fat saturated images. The lesion is best visualized on post-contrast T1-weighted fat saturated images[19]. The only concern about MR scan is the risk of nephrogenic systemic sclerosis due to gadolinium.
The majority of patients with EA recover spontaneously within less than four weeks with conservative management[20]. Recurrence of symptoms have been reported in up to 40% of cases, where surgery in the form of laparoscopic or conventional open excision of the inflamed epiploic appendix may be needed[13]. Establishment of an early and definitive diagnosis of EA may not be straightforward, in PD patients, as it happened in our case. There was a delay of 6 wk before a diagnostic laparoscopy was performed. We believe that a low threshold for diagnostic laparoscopy should be maintained if the symptoms fail to resolve within a week or the diagnosis remains uncertain[21,22]. We did remove the original catheter and used the catheter entry site to introduce a port and telescope. In retrospect, laparoscopy without removal of catheter could have been performed, thereby avoiding the need of removal and replacement of PD catheter.
In a conclusion, establishment of the diagnosis of EA in patients on PD can be challenging, hence a diagnostic laparoscopy should be undertaken early to establish the diagnosis, exclude any other abdominal conditions and retain the PD catheter.
A 67-year-old female, on peritoneal dialysis (PD), presented with recurrent attacks severe left iliac fossa pain.
There was marked tenderness and guarding in the left iliac fossa.
Consideration of acute diverticulitis, appendicitis, haemorrhagic ovarian cyst, torsion of an ovarian cyst, pelvic inflammatory diseases and mesenteric lymphadenitis, delayed perforation of bowel by the PD catheter or ischaemia of intra-abdominal organs, in the differential diagnosis is necessary.
An elevated C-reactive protein was present.
Computed tomography scan of the abdomen showed inflammatory changes in the left iliac fossa (LIF) suggesting the possibility of epiploic appendagitis (EA).
Laparoscopy revealed adhesion of the sigmoid colon to the anterior abdominal wall with an appendix Epiploica was present.
Laparoscopy and adhesiolysis led to complete resolution of symptoms.
Recurrent pain over the LIF is patient on PD in the absence of classical clinical and radiological features should prompt a clinician to consider the diagnosis of EA and perform a diagnostic laparoscopy to establish the diagnosis.
This case report is suitable for publication.
P- Reviewer: Schuld J, Stavroulopoulos A S- Editor: Wen LL L- Editor: A E- Editor: Wu HL
| 1. | Carmichael DH, Organ CH. Epiploic disorders. Conditions of the epiploic appendages. Arch Surg. 1985;120:1167-1172. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 58] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Thomas JH, Rosato FE, Patterson LT. Epiploic appendagitis. Surg Gynecol Obstet. 1974;138:23-25. [PubMed] [Cited in This Article: ] |
| 3. | Sajjad Z, Sajjad N, Friedman M, Atlas SA. Primary epiploic appendagitis: an etiology of acute abdominal pain. Conn Med. 2000;64:655-657. [PubMed] [Cited in This Article: ] |
| 4. | Case TC. Acute epiploic appendagitis. Surgery. 1959;46:1047-1053. [PubMed] [Cited in This Article: ] |
| 5. | Savage L, Gosling J, Suliman I, Klein M. Epiploic appendagitis with acute appendicitis. BMJ Case Rep. 2013;2013. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Son HJ, Lee SJ, Lee JH, Kim JS, Kim YH, Rhee PL, Kim JJ, Paik SW, Rhee JC, Choi KW. Clinical diagnosis of primary epiploic appendagitis: differentiation from acute diverticulitis. J Clin Gastroenterol. 2002;34:435-438. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 44] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Hwang JA, Kim SM, Song HJ, Lee YM, Moon KM, Moon CG, Koo HS, Song KH, Kim YS, Lee TH. Differential diagnosis of left-sided abdominal pain: primary epiploic appendagitis vs colonic diverticulitis. World J Gastroenterol. 2013;19:6842-6848. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 22] [Cited by in F6Publishing: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Kras E, Brun A, Bertrand B, Luigi S. Epiploic appendagitis: a differential diagnosis of acute abdominal pain needing surgery. Presse Med. 2013;42:357-360. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Shrestha BM, Brown P, Wilkie M. Surgical peritonitis in patients on peritoneal dialysis. Perit Dial Int. 2008;28:331-334. [PubMed] [Cited in This Article: ] |
| 10. | Shrestha BM, Wilkie M, Raftery AT. Delayed colonic perforation caused by an unused CAPD catheter in a patient presenting with diarrhea. Perit Dial Int. 2003;23:610-611. [PubMed] [Cited in This Article: ] |
| 11. | Harwell CM, Newman LN, Cacho CP, Mulligan DC, Schulak JA, Friedlander MA. Abdominal catastrophe: visceral injury as a cause of peritonitis in patients treated by peritoneal dialysis. Perit Dial Int. 1997;17:586-594. [PubMed] [Cited in This Article: ] |
| 12. | Cancarini GC, Carli O, Cristinelli MR, Manili L, Maiorca R. Pneumoperitoneum in peritoneal dialysis patients. J Nephrol. 1999;12:95-99. [PubMed] [Cited in This Article: ] |
| 13. | Sand M, Gelos M, Bechara FG, Sand D, Wiese TH, Steinstraesser L, Mann B. Epiploic appendagitis--clinical characteristics of an uncommon surgical diagnosis. BMC Surg. 2007;7:11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 91] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Hasbahceci M, Erol C, Seker M. Epiploic appendagitis: is there need for surgery to confirm diagnosis in spite of clinical and radiological findings? World J Surg. 2012;36:441-446. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Abu-Zidan FM. Epiploic appendagitis: is there a need for surgery to confirm the diagnosis? World J Surg. 2012;36:1449-1450; author reply 1449-1450. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Ozdemir S, Gulpinar K, Leventoglu S, Uslu HY, Turkoz E, Ozcay N, Korkmaz A. Torsion of the primary epiploic appendagitis: a case series and review of the literature. Am J Surg. 2010;199:453-458. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Schnedl WJ, Krause R, Tafeit E, Tillich M, Lipp RW, Wallner-Liebmann SJ. Insights into epiploic appendagitis. Nat Rev Gastroenterol Hepatol. 2011;8:45-49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Singh AK, Gervais DA, Hahn PF, Sagar P, Mueller PR, Novelline RA. Acute epiploic appendagitis and its mimics. Radiographics. 2005;25:1521-1534. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 193] [Cited by in F6Publishing: 165] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 19. | Sirvanci M, Balci NC, Karaman K, Duran C, Karakaş E. Primary epiploic appendagitis: MRI findings. Magn Reson Imaging. 2002;20:137-139. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Schnedl WJ, Krause R, Wallner-Liebmann SJ, Tafeit E, Mangge H, Tillich M. Primary epiploic appendagitis and successful outpatient management. Med Sci Monit. 2012;18:CS48-CS51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |